From conventional epidemiology to systems epidemiology
Conventional epidemiology (sometimes referred to as “black-box epidemiology”) has successfully identified important risk factors (e.g., bronchiolitis, indoor/outdoor environment) for childhood asthma, but it has not illuminated biological mechanisms that undlier the pathogenesis. The lack of understanding has hindered efforts to develop primary prevention strategies for asthma. This major knowledge gap necessitate a paradigm shift from the conventional epidemiology frameworks
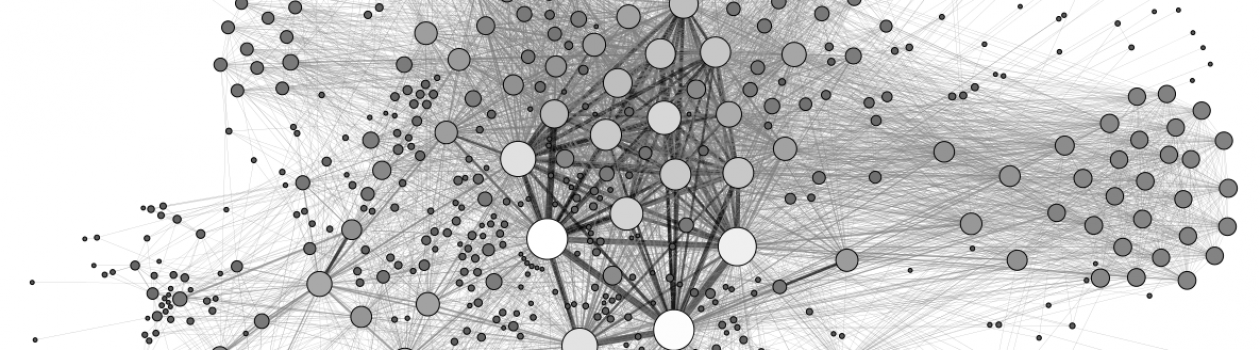
The recent advent of omics technology has enabled us to incorporate molecular data at multiple levels into human observational studies, with the potential to shift the research paradigm from the conventional strategy to a systems approach – systems epidemiology. At the intersection of observational or interventional studies and the concept of systems biology, this new model integrates a wide range of information – e.g., genome, epigenome, transcriptome, proteome, metabolome, microbiome – into high-quality cohort studies with longitudinal assessment of clinical and environmental data. It aims to advance our understanding of the biological mechanisms that underlie complex disease phenotypes.
Our synergistic goals are – through transforming the current framework of bronchiolitis and asthma research into the systems epidemiology approach – 1) to dissect the complex interplay between the host, respiratory viruses, microbiome, and environment, as well as their contributions to the pathobiology of bronchiolitis and asthma; 2) to develop targeted treatment strategies of bronchiolitis; and 3) to develop primary prevention strategies for childhood asthma.